Normal Socket After Tooth Extraction: 2026 Complete Healing Guide with Pictures
When a tooth is removed, your body immediately begins a remarkable healing process. The empty socket…
When a tooth is removed, your body immediately begins a remarkable healing process. The empty socket left behind in your jawbone is a natural part of tooth extraction, and understanding what to expect can help you heal properly and avoid complications. In 2026, with improved dental care protocols and better patient education, most people experience smooth, predictable healing when they follow proper aftercare instructions.
The socket fills with a protective blood clot within hours of extraction, which serves as a natural bandage over the exposed bone and nerve endings. This clot is essential for proper healing and should remain undisturbed during the critical first few days. With appropriate care, your extraction site will progress through predictable healing stages, eventually filling in with new bone and gum tissue over several weeks to months.
Why it helps: Includes sterile gauze, salt rinse packets, and ice packs specifically designed for post-extraction care.
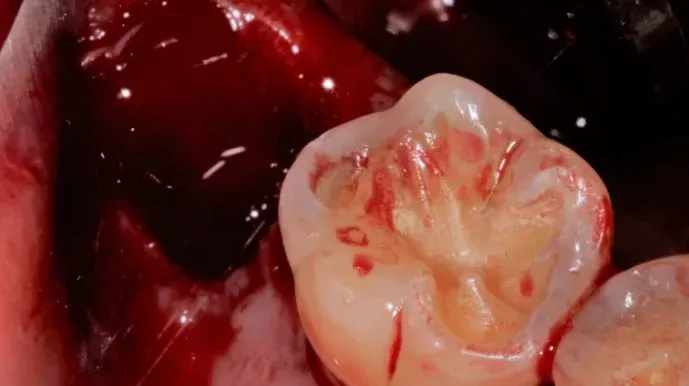
What Does a Normal Socket Look Like After Tooth Extraction?
Immediately following your tooth extraction, the socket will appear as a dark, blood-filled hole where your tooth once was. This is completely normal and expected. The area will be tender, and you may notice some bleeding for the first few hours. Within 24 hours, a dark red or brownish blood clot should form, covering the extraction site.
During the first week, the socket will gradually change appearance as healing progresses. The blood clot may appear whitish or yellowish on the surface—this is normal healing tissue, not infection. The surrounding gum tissue may be slightly swollen and sensitive to touch.
By week two, you should notice the socket beginning to fill in with granulation tissue, which appears pinkish and slightly bumpy. The opening will become smaller as new tissue grows from the bottom up. Most discomfort should be significantly reduced by this point, though some sensitivity when chewing is normal.
After three to four weeks, the socket should be mostly filled with soft tissue, and the gum line will begin to look more normal. Complete bone healing takes three to six months, but you won’t see this process as it happens beneath the gum surface.
Normal Healing Timeline: What to Expect Day by Day
Days 1-2: Expect some bleeding, swelling, and discomfort. The blood clot forms and is extremely fragile. This is the most critical period for avoiding dry socket. Stick to soft foods, avoid rinsing vigorously, and don’t use straws.
Days 3-7: Swelling peaks around day 3 and then gradually decreases. Pain should be manageable with over-the-counter medications. The blood clot becomes more stable, but still requires gentle care. You may notice a white or yellowish film over the socket—this is healthy healing tissue.
Days 7-10: Most acute symptoms resolve. The socket begins filling with granulation tissue. You can gradually return to normal eating habits, though you should still avoid chewing directly on the extraction site.
Weeks 2-4: The socket continues filling in with soft tissue. The opening becomes noticeably smaller. Any remaining discomfort should be minimal.
Months 1-6: Bone remodeling occurs beneath the surface. The gum tissue fully closes over the extraction site. The jawbone gradually fills in the socket with new bone tissue.
Dry Socket vs Normal Healing: Critical Differences
Understanding the difference between normal healing and dry socket (alveolar osteitis) is crucial for recognizing when something has gone wrong. Dry socket occurs in approximately 2-5% of all extractions and is one of the most common complications following tooth removal.
Blood Clot Presence: In normal healing, the protective blood clot remains firmly in place throughout the healing process. With dry socket, this clot either fails to form properly, dissolves prematurely, or becomes dislodged, leaving the bone and nerve endings exposed to air, food, and bacteria.
Pain Characteristics: Normal post-extraction discomfort is typically manageable with standard pain relievers and steadily improves each day. Dry socket pain is distinctly different—it usually begins 2-4 days after extraction and is characterized by severe, throbbing pain that radiates to your ear, eye, temple, or neck on the same side. The pain often worsens rather than improves and may not respond well to typical painkillers.
Why it helps: Antibacterial mouth rinse helps prevent infection and promotes healing after dental procedures.
Visual Appearance: A normally healing socket will have a dark blood clot visible initially, then gradually fill with pinkish-white granulation tissue. The socket with dry socket appears empty—you can often see exposed bone at the bottom, which may appear grayish-white or yellowish. The surrounding gum tissue may look inflamed.
Taste and Odor: Normal healing shouldn’t produce any particularly unpleasant taste or smell beyond what you’d expect from having a wound in your mouth. Dry socket frequently causes a distinctly foul taste and bad breath due to the exposed bone and potential bacterial accumulation in the empty socket.
Healing Duration: Normal extraction sites show steady improvement and are largely healed within 7-10 days for soft tissue. Dry socket significantly delays healing and can cause symptoms for 10-14 days or longer without proper treatment.
Warning Signs of Dry Socket: When to Call Your Dentist
Recognizing dry socket early allows for prompt treatment and faster relief. Contact your dentist immediately if you experience any of these warning signs:
Severe pain that worsens: Instead of gradually improving, your pain intensifies 2-4 days after extraction. This pain is often described as severe, throbbing, and radiating beyond the extraction site. If you’re experiencing persistent pain days after extraction, don’t wait to seek help.
Visible bone in the socket: When you look in the mirror or feel with your tongue, you can see or feel exposed bone instead of a blood clot or healing tissue covering the extraction site.
Bad breath and foul taste: A persistent unpleasant odor or taste that doesn’t improve with gentle rinsing or brushing may indicate dry socket or infection.
Partial or complete loss of the blood clot: If you notice the dark clot that was present initially is now missing or has significantly decreased in size, leaving an empty-looking socket.
Radiating pain: Discomfort that extends to your ear, eye, temple, or neck on the affected side is characteristic of dry socket.
Swollen lymph nodes: Tender, swollen lymph nodes under your jaw or in your neck may indicate infection.
Low-grade fever: A temperature of 99-101°F may suggest your body is fighting an infection at the extraction site.
Is Dry Socket Dangerous?
While dry socket is not life-threatening, it’s a painful complication that requires professional treatment. The exposed bone and nerve endings cause significant discomfort that can interfere with eating, sleeping, and daily activities. Without treatment, the pain can persist for weeks.
The primary concern with dry socket is not the condition itself, but the potential for secondary infection. The exposed bone is vulnerable to bacterial colonization, which can lead to more serious infections if left untreated. In rare cases, untreated infections can spread to surrounding tissues or even into the bloodstream.
The good news is that dry socket is highly treatable. Your dentist will clean the socket, remove any debris, and place a medicated dressing that provides immediate pain relief. Most patients experience significant improvement within 24-48 hours of treatment. The dressing may need to be changed every few days until healing progresses normally.
In 2026, dentists may also use advanced treatments such as platelet-rich fibrin (PRF) or growth factors to accelerate healing in dry socket cases. These biological materials help stimulate tissue regeneration and reduce recovery time.
Proper Aftercare for Normal Socket Healing
Following your dentist’s post-operative instructions carefully is the best way to ensure normal healing and avoid complications like dry socket. Here are the essential aftercare guidelines for 2026:
First 24 Hours:
- Bite firmly on gauze for 30-45 minutes to allow clot formation
- Apply ice packs to the outside of your face (20 minutes on, 20 minutes off) to reduce swelling
- Avoid rinsing, spitting, or using straws—the suction can dislodge the clot
- Rest with your head elevated on pillows
- Stick to cold, soft foods like yogurt, smoothies, and ice cream
- Take prescribed pain medications as directed
- Don’t smoke or use tobacco products
Days 2-7:
- Begin gentle salt water rinses after 24 hours (½ teaspoon salt in 8 oz warm water) 4-6 times daily
- Continue soft diet, gradually introducing more solid foods as tolerated
- Brush teeth carefully, avoiding the extraction site
- Continue avoiding smoking, straws, and vigorous rinsing
- Apply warm compresses to reduce swelling
- Stay hydrated but avoid alcohol and carbonated beverages
Why it helps: Flexible gel packs conform to your jaw and provide consistent cold therapy to reduce swelling and pain.
Week 2 and Beyond:
- Resume normal oral hygiene, being gentle around the healing site
- Gradually return to your regular diet
- Continue salt water rinses after meals until fully healed
- Attend any scheduled follow-up appointments
Foods to Eat and Avoid During Healing
Best Foods for the First Week:
- Yogurt and smoothies (no straws)
- Mashed potatoes and soft-cooked vegetables
- Scrambled eggs
- Oatmeal and cream of wheat
- Soup (lukewarm, not hot)
- Protein shakes
- Soft fruits like bananas and avocados
- Pudding and applesauce
Foods to Avoid:
- Crunchy foods (chips, nuts, popcorn)
- Hard or chewy foods (steak, bagels, candy)
- Small seeds or grains that can lodge in the socket
- Spicy foods that may irritate the site
- Very hot foods or beverages
- Alcohol and carbonated drinks
- Acidic foods and drinks
When to Contact Your Dentist
While some discomfort is normal after tooth extraction, certain symptoms warrant immediate professional attention. Contact your dentist if you experience:
- Severe pain that doesn’t respond to prescribed medications
- Heavy bleeding that doesn’t stop after 4 hours of applying pressure
- Fever above 101°F
- Difficulty swallowing or breathing
- Excessive swelling that worsens after 3 days
- Numbness that persists beyond the expected duration of anesthesia
- Pus or discharge from the extraction site
- Signs of allergic reaction to medications
Long-Term Considerations After Tooth Extraction
Once your extraction site has healed, you may need to consider tooth replacement options to maintain proper jaw alignment and function. Missing teeth can cause neighboring teeth to shift, affect your bite, and lead to bone loss in the jaw over time.
Modern tooth replacement options in 2026 include dental implants, bridges, and partial dentures. Dental implants are considered the gold standard as they replace both the tooth root and crown, helping preserve jawbone density. Your dentist can discuss which option is best for your specific situation.
Even if you don’t immediately replace the tooth, maintaining excellent oral hygiene and regular dental checkups is essential for preventing future tooth loss and maintaining overall oral health.
Conclusion: Ensuring Successful Healing
A normal socket after tooth extraction should heal predictably and with manageable discomfort when you follow proper aftercare instructions. The key to successful healing is protecting that crucial blood clot during the first few days, maintaining good oral hygiene, and watching for warning signs of complications.
Remember that healing is a gradual process that takes weeks to months for complete bone regeneration. Be patient with your body, follow your dentist’s instructions carefully, and don’t hesitate to reach out if something doesn’t feel right. With proper care, your extraction site will heal completely, leaving you with a healthy foundation for whatever comes next—whether that’s a replacement tooth or simply maintaining the space.
If you’re concerned about any aspect of your healing process, your dentist is your best resource for personalized guidance and treatment. Early intervention for complications like dry socket can make a significant difference in your comfort and recovery time.