Tooth Abscess Still Swollen After 3 Days of Antibiotics? Here’s What to Do in 2026
A tooth abscess can be an excruciatingly painful dental condition that demands prompt attention and treatment….
A tooth abscess can be an excruciatingly painful dental condition that demands prompt attention and treatment. When your dentist prescribes antibiotics to combat the infection causing the abscess, you might expect relief within a few days. However, if your tooth abscess is still swollen after three days of antibiotics, it can be a cause for concern. In this comprehensive guide, we’ll explore why a tooth abscess may remain swollen despite antibiotic treatment, what steps you can take, when to seek professional help, potential complications of an untreated abscess, and strategies for preventing its recurrence.
Why it helps: Contains essential tools for managing abscess discomfort at home while waiting for professional treatment.
What to Do If Your Tooth Abscess Is Still Swollen After 3 Days of Antibiotics
If your tooth abscess is still swollen after three days of antibiotics, it’s essential to take the following steps to address the situation:
- Continue Antibiotics: Complete the full course of antibiotics as prescribed by your dentist. Do not stop taking them prematurely, even if you haven’t experienced significant improvement in swelling. Antibiotics need time to combat the infection effectively, and stopping early can lead to antibiotic resistance.
- Pain Management: Over-the-counter pain relievers can help manage the discomfort associated with a swollen abscess. If you’re experiencing severe tooth pain that’s keeping you awake, consider using a combination approach under your dentist’s guidance. Follow the recommended dosage instructions on the medication label.
- Maintain Oral Hygiene: Continue to practice good oral hygiene, including gentle brushing and flossing, while avoiding the affected area. Keeping your mouth clean can prevent further complications and support the healing process.
- Warm Saltwater Rinse: Rinse your mouth with warm saltwater (one teaspoon of salt dissolved in eight ounces of water) several times a day. This can help reduce inflammation and cleanse the affected area naturally.
- Avoid Aggravating Foods: Stick to a soft diet and avoid hot, cold, spicy, or crunchy foods that may worsen the pain or swelling. Opt for lukewarm soups, smoothies, and soft proteins during recovery.
- Elevation: If swelling is present on the outside of your face, you can use a cold compress or ice pack wrapped in a cloth to reduce it. Apply the compress in 15-minute intervals, making sure not to apply it directly to the skin to prevent tissue damage.
Is It Normal for a Tooth Abscess to Still Be Swollen After 3 Days of Antibiotics?
While it’s common to expect some improvement in swelling and discomfort within three days of antibiotic treatment, it’s not unusual for a tooth abscess to still be swollen after this time frame. Several factors can influence the rate of improvement and resolution, including:
- Size and Severity: The size and severity of the abscess can significantly impact the time it takes for the swelling to decrease. Larger or more severe abscesses may require a longer recovery period, sometimes extending to 7-10 days or more before noticeable improvement occurs.
- Effectiveness of Antibiotics: The type of antibiotics prescribed and the susceptibility of the bacteria causing the infection can affect the speed of improvement. Some infections may require a specific antibiotic regimen or a longer treatment duration. In 2026, your dentist may use advanced bacterial testing to identify the most effective antibiotic for your specific infection.
- Individual Response: Everyone’s body reacts differently to infections and antibiotics. Some individuals may experience rapid improvement, while others may take longer to see results based on their immune system strength, overall health, and medication metabolism.
- Biofilm Formation: Bacterial biofilms can form around the infection site, making it harder for antibiotics to penetrate and eliminate the bacteria completely. This is one reason why antibiotics alone may not resolve the abscess without additional dental intervention.
While it’s normal for improvement to take time, it’s crucial to monitor your condition closely and seek professional help if the swelling persists, worsens, or if you develop new symptoms like fever or difficulty swallowing.
Why it helps: Monitor your temperature to detect if the infection is spreading systemically, requiring immediate medical attention.
When Should I See a Dentist If My Tooth Abscess Is Still Swollen After 3 Days of Antibiotics?
If your tooth abscess remains swollen after three days of antibiotics, you should contact your dentist for a follow-up appointment. Your dentist will evaluate your condition and may take the following steps:
- Reassessment: The dentist will examine the abscess, assess the degree of swelling, and determine if there is any pus accumulation. They’ll also check for signs that the infection is spreading to surrounding tissues.
- Adjust Antibiotics: Depending on your progress, the dentist may choose to modify your antibiotic prescription. They may prescribe a different type, increase the dosage, or continue the current course if they believe it is still effective but needs more time to work.
- Possible Drainage: In cases where there is significant pus accumulation, the dentist may need to drain the abscess to relieve pressure and facilitate healing. This procedure, called incision and drainage, can provide immediate relief and help antibiotics work more effectively.
- Radiographs: X-rays or other imaging may be taken to assess the extent of the infection and to determine if there are any underlying issues, such as an impacted tooth, bone loss, or a periapical lesion that requires additional treatment.
- Root Canal or Extraction: Antibiotics alone cannot cure a tooth abscess—they only control the infection temporarily. Your dentist will likely recommend definitive treatment such as a root canal to save the tooth or extraction if the tooth cannot be saved. Understanding the dangers of pulling an abscessed tooth can help you make an informed decision about your treatment options.
- Referral: In complex cases or if there are complications, your dentist may refer you to an oral surgeon or endodontist for specialized treatment.
Seek immediate emergency care if you experience:
- Difficulty breathing or swallowing
- High fever (over 101°F or 38.3°C)
- Rapid swelling that extends to your neck or eye area
- Severe pain that doesn’t respond to medication
- Confusion or altered mental state
What Are the Complications of a Tooth Abscess That Is Not Treated?
Failing to address a tooth abscess promptly can lead to various serious complications, including:
- Spread of Infection: The infection can extend beyond the tooth and abscess site, affecting nearby structures like bone, neighboring teeth, and even the bloodstream. This can lead to osteomyelitis (bone infection) or damage to adjacent teeth.
- Cellulitis: Untreated abscesses can result in cellulitis, a painful bacterial skin infection that can spread rapidly through facial tissues, causing significant swelling and redness.
- Ludwig’s Angina: In severe cases, infection can lead to Ludwig’s angina, a potentially life-threatening condition characterized by swelling and infection of the floor of the mouth and throat. This can obstruct airways and requires emergency medical intervention.
- Systemic Infection (Sepsis): In rare but serious cases, bacteria from an untreated tooth abscess can enter the bloodstream, causing sepsis, a severe and potentially fatal infection that affects the entire body. Understanding how quickly a tooth infection can become life-threatening emphasizes the importance of prompt treatment.
- Brain Abscess or Meningitis: Though extremely rare, bacteria from a dental abscess can spread to the brain, causing brain abscess or meningitis, both of which are medical emergencies requiring immediate hospitalization.
- Chronic Infection: Long-term neglect of a tooth abscess can lead to chronic, persistent infection, which can result in ongoing pain, discomfort, and recurrent swelling that becomes increasingly difficult to treat.
- Loss of Tooth: In many cases, an untreated abscess will lead to tooth loss, as the infection damages the supporting structures of the tooth, including the periodontal ligament and surrounding bone.
- Sinus Complications: Upper tooth abscesses can spread into the maxillary sinuses, causing chronic sinusitis and persistent facial pain.
How to Prevent a Tooth Abscess from Recurring
Preventing a tooth abscess from recurring or developing in the first place is essential for maintaining oral health. Here are some evidence-based steps you can take to minimize the risk:
- Maintain Good Oral Hygiene: Brush your teeth at least twice a day with fluoride toothpaste, floss daily, and use an antiseptic mouthwash. Proper oral hygiene can help prevent tooth decay and gum disease, which are the primary causes of dental abscesses.
- Regular Dental Checkups: Schedule regular dental checkups and cleanings every six months to detect and address dental issues before they escalate. Early intervention can prevent cavities from progressing to abscesses.
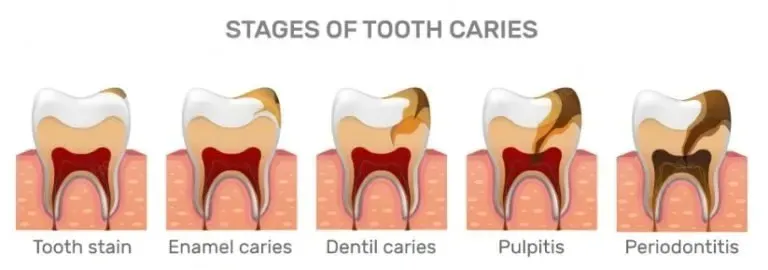
- Address Cavities Promptly: If you have cavities, get them filled promptly to prevent the spread of decay into the tooth’s pulp, which can lead to abscess formation.
- Complete Recommended Treatments: If your dentist recommends a root canal or crown, follow through with the treatment. Delaying necessary dental work can allow infections to develop or worsen.
- Practice Safe Dental Care: Avoid habits that can damage your teeth, such as chewing on hard objects, using your teeth to open packages, or grinding your teeth at night. If you grind your teeth, consider getting a night guard for teeth grinding to protect your enamel.
- Manage Dry Mouth: If you have dry mouth (xerostomia), take steps to manage it, as reduced saliva flow can increase the risk of tooth decay. Stay hydrated, use saliva substitutes, and avoid alcohol-based mouthwashes.
- Balanced Diet: Consume a balanced diet low in sugary and acidic foods to promote healthy teeth. Limit snacking between meals and rinse your mouth with water after consuming sugary or acidic foods.
- Wear Protective Gear: If you engage in contact sports or activities with a risk of dental injury, wear a properly fitted mouthguard to protect your teeth from trauma that could lead to infection.
- Address Gum Disease: Gum disease can create pockets where bacteria accumulate, leading to periodontal abscesses. If you notice signs of gum disease, seek treatment promptly.
- Avoid Smoking: Smoking weakens your immune system and increases your risk of dental infections. Quitting smoking can significantly improve your oral health and reduce abscess risk.
Why it helps: Reduces bacterial load in your mouth and helps prevent future infections when used as part of your daily oral hygiene routine.
Understanding Why Antibiotics Alone Aren’t Enough
It’s important to understand that antibiotics are not a cure for a tooth abscess—they’re a temporary measure to control the infection. Here’s why:
- Source Remains: The source of the infection (decayed tooth tissue or infected pulp) remains inside the tooth. Antibiotics can’t penetrate deep enough into the tooth to eliminate the bacteria at the source.
- Limited Blood Supply: Abscessed teeth often have compromised blood supply, which means antibiotics delivered through your bloodstream may not reach the infection site effectively.
- Biofilm Protection: Bacteria in dental abscesses form protective biofilms that shield them from antibiotics, making it difficult for medication alone to eliminate the infection completely.
- Recurrence Risk: Without definitive treatment (root canal or extraction), the infection will almost certainly return once you stop taking antibiotics, often becoming more resistant to treatment.
This is why your dentist will emphasize the need for follow-up treatment even if the antibiotics seem to be working. The medication buys time and reduces acute symptoms, but it doesn’t solve the underlying problem.
Conclusion
Experiencing a swollen tooth abscess after three days of antibiotic treatment can be distressing, but it’s not uncommon. The key is to remain vigilant, follow prescribed treatments completely, and seek professional dental care if the swelling persists or worsens. Remember that antibiotics alone cannot cure a dental abscess—they only control the infection temporarily until definitive treatment can be performed.
Timely intervention and proper management can help resolve the abscess, alleviate discomfort, and prevent potentially severe complications. In 2026, with advances in dental technology and treatment protocols, your dentist has more tools than ever to diagnose and treat abscesses effectively. Additionally, maintaining good oral hygiene and adopting preventive measures can significantly reduce the risk of future tooth abscesses, ensuring a healthier and pain-free smile.
If you’re currently dealing with a persistent abscess, don’t wait—contact your dentist immediately to discuss your symptoms and next steps. Your oral health is too important to delay, and prompt professional care can make all the difference in your recovery and long-term dental wellness.